POROUS AND NON-POROUS IMPLANTS
(by R. Angeli, University of Milano-Bicocca, 2005)
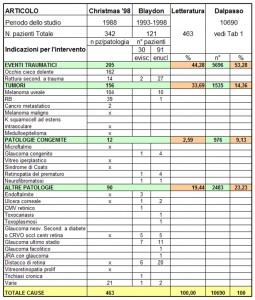
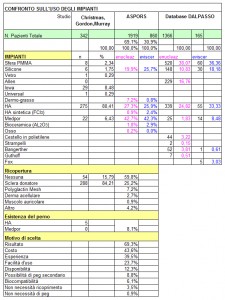
The comparison between DALPASSO records and ASPORS (American Society of Ophthalmic Plastic and Reconstructive Surgery) files highlights some differences.
While ASPORS mainly uses porous implants, DALPASSO clearly opts for non-porous ones.
As for porous implants, ASPORS uses Medpor and hydroxyapatite respectively in 42.5% and 26.6% of both evisceration and enucleation cases; on the contrary, DALPASSO opts for hydroxyapatite in 24.8% of enucleation cases and in 33.3% of evisceration ones, and for Medpor in just 1.8% of enucleation cases and in 8.5% of evisceration ones.
As for non-porous implants, DALPASSO works with silicone in 10.8% of enucleation cases and in 18.2% of evisceration ones, and with PMMA in 38.1% of enucleation cases and in 36.4% of evisceration ones; on the other hand, ASPORS makes no distinction between silicone and Medpor, so it uses a non-porous material in 19.9% of enucleation cases and in 25.7% of evisceration ones.
Consequently, these data reveal that Italian cases occurred over the last decades were solved mostly by means of non-porous implants.
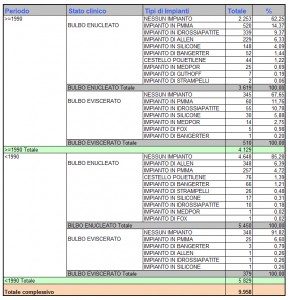
In DALPASSO records, year 1990 represents the cut-off chosen to split time in two periods of analysis. It allows to study the evolution of orbital implants underlining the growing importance of porous ones.
Despite non-porous implants prevail, indeed, the increasing number of porous ones proves that they have definitely turned to be a valid alternative.
This cut-off, however, limits the analysis itself to what happened right before and after 1990, not allowing a more precise examination of the most recent years. This may be one of the reasons why the percentage of porous implants use is lower than the non-porous one.